Magnetic Moments is a series of stories that highlight the high quality care and experience that makes Mount Sinai Hospital the only hospital in Canada to have Magnet™ designation.
Regular news reports of the opioid crisis has sparked a discussion around safe approaches to pain management. But how do we ensure this when it comes to managing pain after a surgery?
The prescription of opioids is a common practice to help patients manage post-operative pain, but Mount Sinai Hospital was seeing up to six patients a week with complex pain histories, chronic pain or even chronic opioid use. For these patients, using opioids to manage pain was not necessarily appropriate – resulting in some patients waking up after surgery in pain crises.
With the goal of improving their experience, Giuliana Vertolli and Jaclyn Ricci, nurse practitioners in the Acute Pain Service set out to establish a new organizational practice that highlighted the potential benefits of ketamine therapy for patients with difficult to treat post-operative pain.
“Ketamine was seen by the care team as a last resort, an old approach to managing pain.” says Jaclyn. “This was a medication that for our 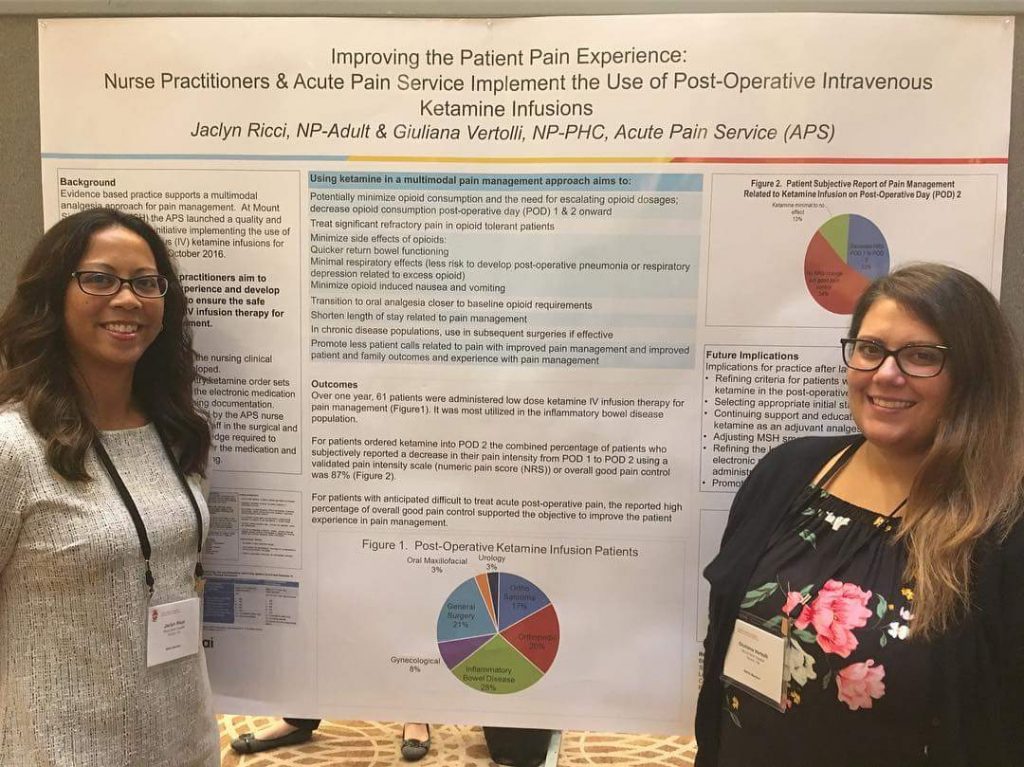 inpatients was only used in our intensive care unit. We spent a lot of time listening to the team and put a focus on education to ensure the care team felt confident in administering the medication.”
inpatients was only used in our intensive care unit. We spent a lot of time listening to the team and put a focus on education to ensure the care team felt confident in administering the medication.”
And their work to educate the team shows. “Sinai Health has always been at the forefront in revolutionizing the way we manage pain. When Ketamine was introduced, the education was seamlessly provided to ensure our nurses were well equipped to embed this new methodology into their practice,” says Sarabeth Silver, Clinical Nurse Specialist, in surgical oncology.
Jaclyn and Giuliana also worked to proactively identify patients that could benefit from this pain management approach. Some of the benefits of using intravenous ketamine include: decrease opioid consumption post-surgery, decreased length of stay related to pain management and improved patient and family experience.
“Since we started using ketamine to help our most complex pain patients, we’ve had 87 per cent reporting good pain control,” notes Giuliana.
So what’s next? Jaclyn and Giuliana are sharing the good results of this pain management protocol. They have presented at the Nurse Practitioner Association of Ontario, shared their knowledge with colleagues at Sunnybrook (who implemented IV ketamine use in August) and are now focusing on expanding to other pain services to ensure access is equitable to all pain patients.
