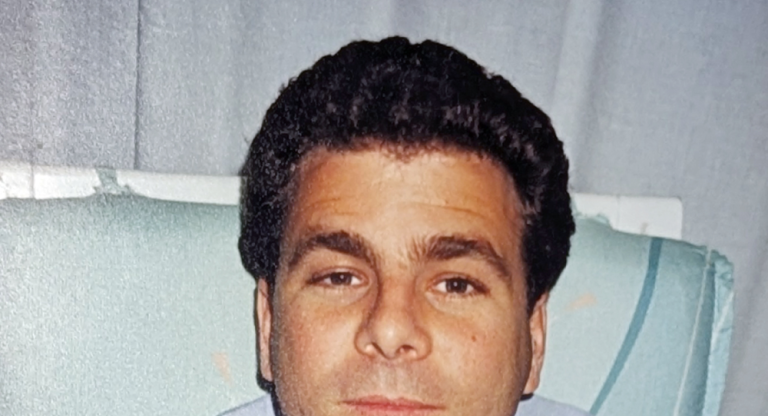
Defying the odds: Mr. Solomon’s return home

Last spring, Mr. Solomon arrived at Mount Sinai Hospital in serious poor health. After many months of cycling through hospitals and rehab centres, he could no longer walk or perform routine daily activities, like getting dressed — and no one could tell him why. He was even being considered for long-term care — a devastating outcome for someone just 62 years old and previously living independently.
“When he was admitted initially, they couldn’t yet explain his condition and he was rapidly losing his functional capabilities,” says Gabriel Chow, Patient Care Manager for Mount Sinai’s 12 South General Internal Medicine Unit.
Mr. Solomon spent the next five months in acute care, much of it in isolation to reduce the risk of infection to others. Eventually, he was diagnosed with POEMS syndrome — a rare, complex blood condition that can cause progressive nerve damage, bone lesions and hormonal imbalances. He’d also experienced multiple strokes, further compounding his mobility issues. Extended time in bed left him with severe foot drop in both feet — a condition that often prevents people from walking again.
“With such severe foot drop, you don’t expect someone to ever walk again,” explains Gabriel. “But Mr. Solomon was eager to participate in his care. Even with all the uncertainty, he gave it everything he had.”
A breakthrough driven by determination
Motivated by his desire to live independently again, Mr. Solomon made slow progress — but he needed intensive rehabilitative care to help him achieve his goal of getting back home. Despite best efforts from his team at Mount Sinai, he was turned down by several community rehab facilities, with the prospect of long-term care looming.
His team believed in his potential and continued to rally behind Mr. Solomon. With the care, support and advocacy from physiatrists, physical and occupational therapists and neurology specialists, Mr. Solomon began to make small and meaningful gains. With customized assistive devices, he began to regain some abilities to participate in activities of daily living, such as feeding himself. He also began to regain some mobility. Then came a breakthrough.
“The team was huddled at the nursing station when we saw Mr. Solomon walking down a hallway we weren’t sure he’d ever walk again,” recalls Gabriel. “In that moment, the station erupted with cheering and clapping. After five months in isolation in acute care, seeing him turn that corner was so encouraging — it was unforgettable.”
That milestone paved the way for Mr. Solomon’s transfer to Hennick Bridgepoint Hospital to continue his rehabilitation.
Connected care guides every step to recovery
The team at Hennick Bridgepoint was ready to build on the fragile progress that Mr. Solomon had made — and help him reach for independence.
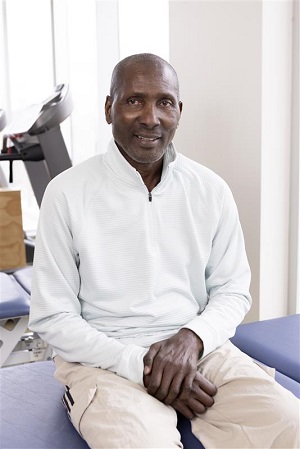
“There was a spark in him,” says Kathleen Reid, RN and Patient Care Manager for the Medical Rehabilitation and Acquired Brain Injuries Units at Hennick Bridgepoint. “He was highly motivated — and that’s so important in rehab.”
Though still unable to feed himself or walk even with aids, Mr. Solomon immersed himself in therapy. “He didn’t want his illness to define him,” says Kathleen. “Even when progress was slow, he stayed hopeful.”
Hennick Bridgepoint’s collaborative care model ensures an integrated, team-based approach to complex care. For patients like Mr. Solomon, that means every part of the care journey — physical recovery, cognitive rehabilitation and emotional wellness — is connected.
His team treated not just his mobility issues, but the whole person: building his strength, helping him regain memory and speech, and preparing him to live independently again. His family’s support was critical — and so was the team’s belief in his potential.
“He had been in and out of rehab for years,” Kathleen explains. “This time, we wanted to go deeper to help him get home and not return to the hospital, unless there's an acute event we can't predict.”
Going home — and staying home
In February, Mr. Solomon was discharged, ending a 10-month journey through the Sinai Health network. As an outpatient, he continues therapy at Hennick Bridgepoint, supported by a team already familiar with his story.
“One of the things that sets us apart from other complex rehabilitation centres in the city is our outpatient therapy department,” says Kathleen. This enables teams at Hennick Bridgepoint to have more direct communication about Mr. Solomon’s full care journey — a perspective otherwise lost if he was referred to an external outpatient clinic.
Now, Mr. Solomon is working on regaining his memory, reading ability and upper body strength. Thanks to therapy, he can now transfer from wheelchair to bed himself and move safely around his home.
To help Mr. Solomon stay independent and safe in his home, he connected to Circle of Care services through the relatively new Sinai Health to Home program. This transitional, home-based program provides highly personalized, enhanced support to eligible patients with complex needs. The program has helped Mr. Solomon make the transition back home, with its focus on integration between Hospital, primary care, home care and community support services. Tools like a fall-detecting pendant and medication alarms further help him live safely and as independently as possible.
Mr. Solomon’s story is a reminder of what integrated care makes possible. It’s about more than medicine — it’s about seeing the whole person, understanding what matters most to them and pulling together every available resource to help them live the life they imagine for themselves.
“Mr. Solomon reminded us of why we do this,” Kathleen says. “We were able to help him not just recover but return to the community on his terms.”
Help get the next patient home
“While I have trouble remembering the details of my experience, I am so appreciative of all the help from my health-care teams, and those who choose to support Sinai Health,” shares Mr. Solomon.
Your generosity drives the programs, the teams and the patient-centred approach that turn “unlikely” outcomes into real, life-changing recoveries. Donate today — and help the next patient get home.