Healing beyond survival: Sinai Health’s leading-edge research into breast cancer recovery
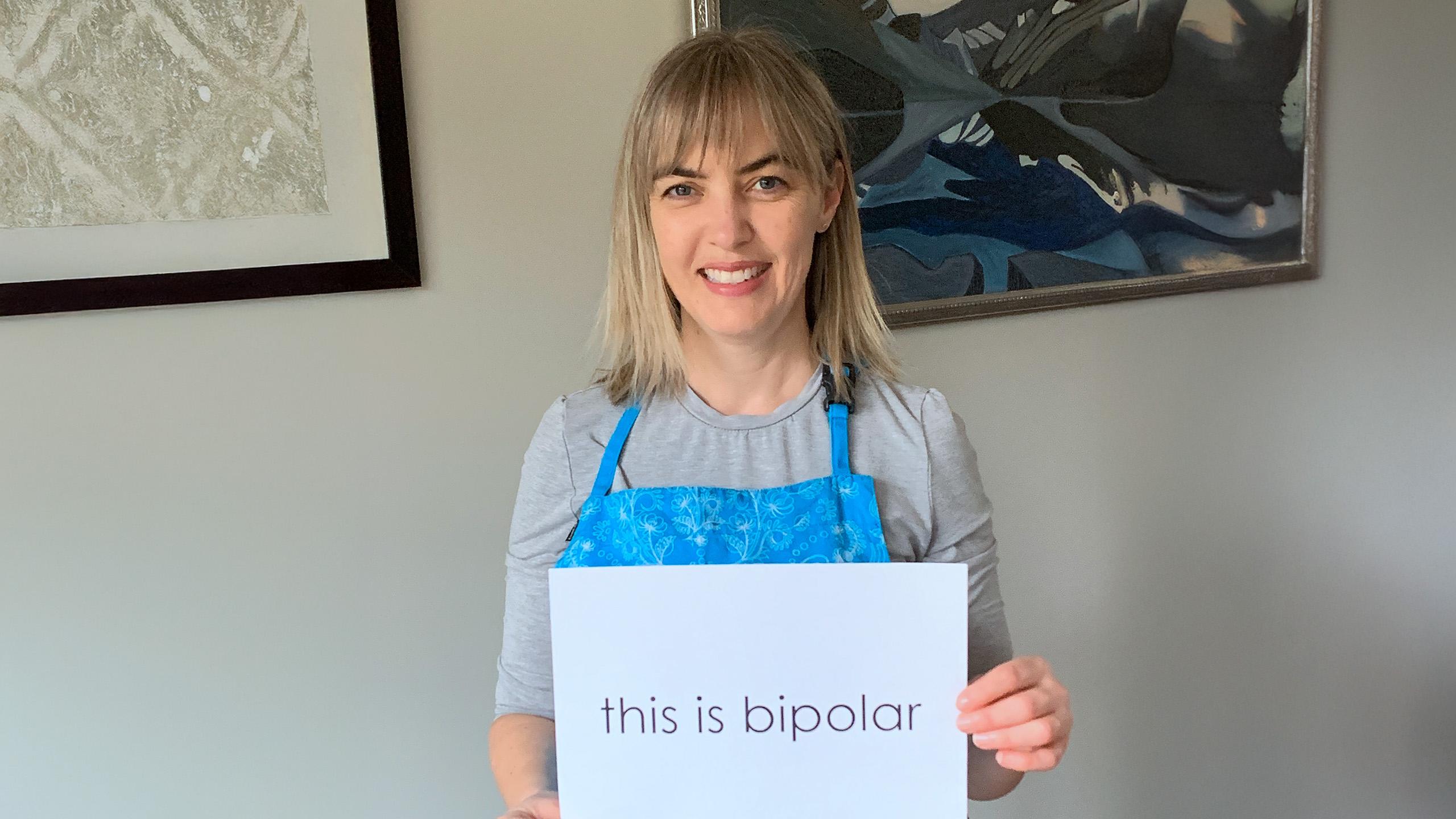
With Breast Cancer Awareness Month already underway, Deborah Peniuk’s story is a powerful reminder that for many survivors, the challenges don’t end when treatment does.
When Deborah was diagnosed with breast cancer 10 years ago, she steeled herself for what lay ahead: chemotherapy, surgery and radiation. What she didn’t expect was that long after her treatments ended, pain would continue to shadow her daily life.
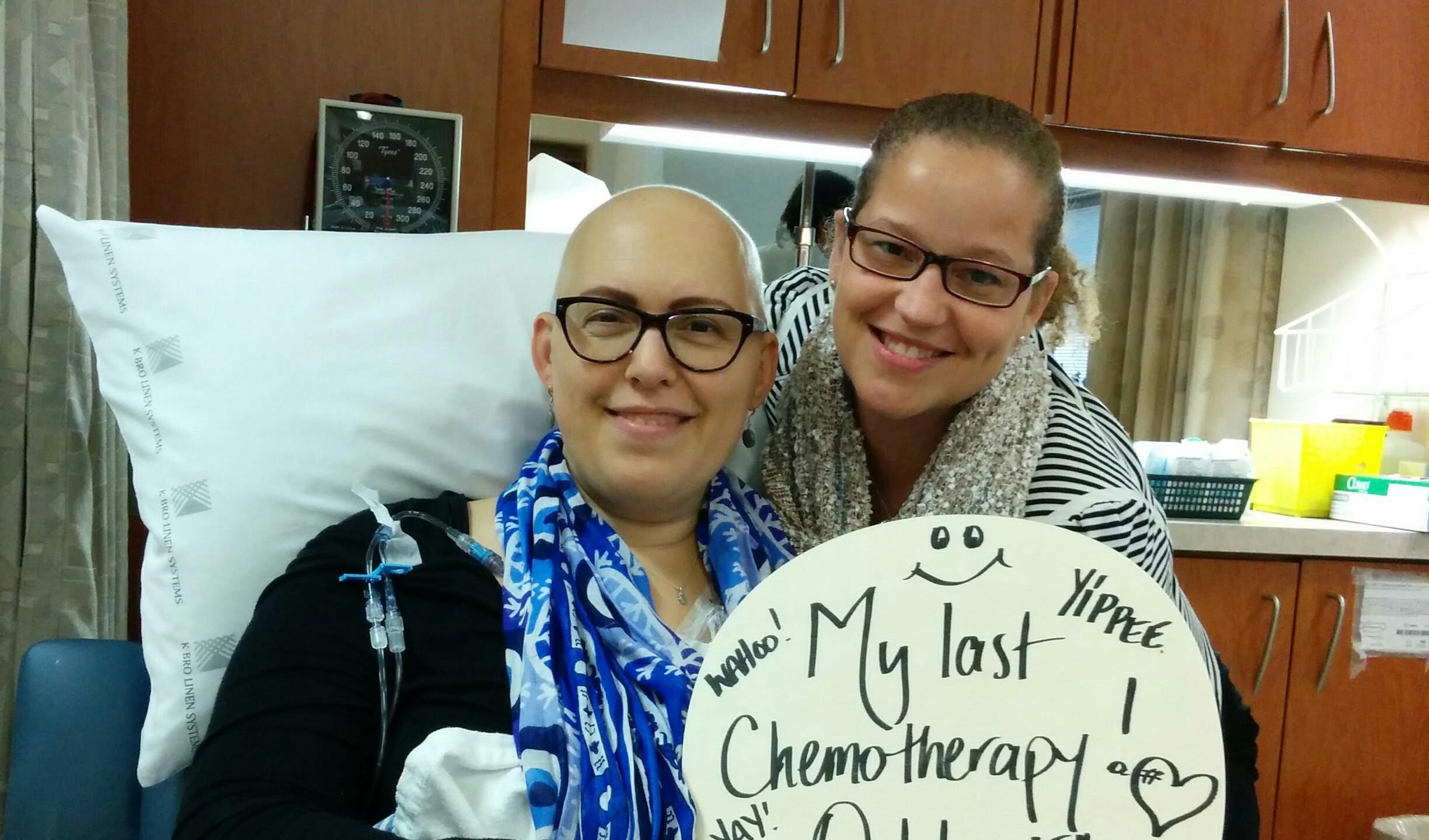
After eight rounds of chemotherapy, a lumpectomy and lymph node dissection, and 30 rounds of radiation, Deborah developed lymphedema, a common side effect of breast cancer treatment, occurring when the removal or damage of lymph nodes disrupts the body’s ability to drain lymph fluid, leading to pain and swelling. “I found it really frustrating to navigate pain management post-treatment,” she recalls. “I knew there were going to be side effects somewhere down the road, but I had no idea where it was going to lead me.”
Deborah tried to find solutions within the health-care system, but her concerns were frequently dismissed, and she was left without answers. “I experienced a lot of health professionals telling me, ‘We don't know, so basically, you're going to have to learn how to live with it.’”
In addition to the lymphedema, Deborah was also suffering from chemo-induced pleural neuropathy, a kind of nerve damage in her hands and feet, and what began as tenderness around her surgical drain site had evolved into an ache that radiated through her chest, arm and back.
A years-long search for answers
For years, Deborah worked to rebuild a sense of normalcy in her day-to-day life. “I wanted to feel whole all over,” she says. “When a particular part of you is not feeling whole, it has a damaging effect on the rest of you.”
For Deborah, part of being whole means making time for activities that bring her joy. She started dragon boating with a breast cancer survivor team, but constant pain soon got in the way. “I had to confront the fact that it was more than just the paddling giving me pain,” she says. “So, I really needed to figure out what I was going to do, because there had to be someone able to help me.”
Unwilling to accept that her pain was permanent, Deborah kept searching for answers. “It took me pushing my surgeon and my GP, saying, I need to figure this out,” she says. Her persistence paid off when she received a referral to Dr. James Khan, chronic pain specialist and Clinician-Scientist, whose research focuses on identifying new interventions to prevent and treat long-term pain. He currently directs Sinai Health’s Persistent Breast Cancer Pain Clinic — the only one of its kind in Canada.
“When I first met Dr. Khan,” says Deborah, “I felt validated because finally someone believed me, and for the first time the pain I was talking about was being received as something that might be solvable.”
Advancing research to transform women’s lives
The Persistent Breast Cancer Pain Clinic is pioneering a new way of understanding and treating post-surgical pain — one that recognizes it as a critical, ongoing part of survivorship care.
Dr. Khan’s work bridges clinical care and research. By studying how pain develops — and how it can be prevented — his team is changing what recovery looks like for women, following breast-cancer surgery. Through the PLAN Trial, an international study involving more than 1,600 patients, Dr. Khan and his collaborators are investigating whether a simple, low-cost lidocaine infusion given during surgery can prevent chronic pain before it starts.
“If the results are positive, the impact could be massive,” says Dr. Khan. “Anesthesiologists and surgeons could adopt these infusions as standard practice, improving quality of life for countless breast cancer survivors at virtually no added cost.”
As she had already undergone surgery, Deborah was not eligible for the PLAN Trial when she met with Dr. Khan. However, the Persistent Breast Cancer Pain Clinic also conducts post-surgical trials, including the one Deborah is involved in. She receives targeted nerve treatments, including cortisone injections and radiofrequency ablation, a medical procedure that uses high-frequency electrical currents to treat pain.
After beginning treatment with Dr. Khan, Deborah experienced real relief for the first time in years. She says it’s been freeing to live without the constant burden of managing her pain. “Receiving treatment that is keenly attuned to the spots where I’m having pain makes such a difference, not only for my body, but also for my mind.”
What’s more, Deborah has resumed dragon boating. “Not having daily, persistent pain has meant being able to rejoin my team more consistently out on the water, paddling even stronger.”

Leading through innovation and compassion
For patients like Deborah, Dr. Khan’s compassion and genuine effort to understand their experience have made all the difference in their lives. “He’s able to personalize conversations, which makes me feel recognized,” she says. “I'm his patient, but he talks to me as an equal, as a human being. And that, I’d say, is not consistent across medical care.”
That human connection — paired with leading-edge research — is what makes Sinai Health’s approach so powerful. “Historically, women’s health questions just haven’t been prioritized the way they should,” Dr. Khan says. “I hope our clinic and research normalize asking women about pain, believing them and doing something about it.”
By challenging the long-standing assumption that women’s pain after breast cancer surgery is “just part of recovery,” Dr. Khan hopes to help save patients from years of suffering. “With chronic pain, women are disproportionately affected, but so much of the data we’ve relied on came from studies in very different populations. We need to generate answers that reflect women’s biology and lived experience.”
For Deborah, being part of research with potential global impact has become a passion. She has participated in multiple research studies — from pain management to genetics — and sees it as a way to pay her experience forward. “I know I'm only one number among many, but I wanted to participate, to feel like I’m helping other women,” she says. “While participating in studies may not benefit me in my lifetime, it's going to benefit someone else. That's just how I live my life, for the most part.”
Turning pain into purpose and driving change in women’s health
As October marks Breast Cancer Awareness Month, Deborah hopes her story will shine a light on the persistent pain that too many survivors endure, an often-overlooked part of recovery. She has also turned her own journey into advocacy. She now mentors other cancer survivors, helping them navigate the health system, connect with resources and feel empowered to ask questions.
“You have to use your voice. You have to peck away at things to try and find answers,” she says. “If I’m able to share what I’ve learned with more people about the power of self-advocacy, I will always take that opportunity.”
Her advice for others living with persistent pain? “Never accept that no is the answer. You don’t have to suffer in silence.”
You can help advance research leading to better outcomes for breast cancer survivors
As a leader in driving critical breakthroughs in women’s health, Sinai Health is helping close long-held gaps in our understanding of how women experience disease and conditions differently from men.
Through clinical innovation and compassion, Dr. Khan’s work — and the generosity of donors supporting research at Sinai Health — is redefining what breast cancer recovery can be. With your ongoing support, we can continue to advance the boundaries of innovation to help more patients like Deborah not only survive, but live pain-free. Donate today.