Mental health care in action: How Charise found support for bipolar disorder at Sinai Health
Charise Jewell was 40 years old and living in Calgary when she started to struggle with insomnia that was more intense than anything she’d ever experienced before. But she didn’t think her sleeplessness was anything to be concerned about.
“For about two or three weeks, I would fall asleep for two or three hours. But then the next day I’d be really productive and functioning at high energy. At first, I was feeling wonderful,” says Charise.
“But as time passed, my husband noticed that I was getting more irritable and confused. Then, I started to have delusions and hallucinations. I was terrified of everything. So, my husband took me to our local emergency department.”
What Charise was experiencing is called mania – an episode characterized by abnormally elevated, extreme changes in one’s mood or emotions that stand out to those around them. It’s a common symptom of bipolar disorder.
Charise was admitted to the psychiatric ward as an inpatient, where she stayed for two weeks. She was diagnosed with bipolar 1 mood disorder and her health team introduced medications to help manage her symptoms. However, her hospitalization was mentally and emotionally challenging. She struggled with confusion and depression.
“I worried about what this would mean for my family. I didn’t know how it would affect my kids or how I could show up for them as a mom,” says Charise. “Everyone made it sound like it was this horrible thing.”
Some of her experiences as an inpatient left her feeling as though she couldn’t fully trust her care team or that her concerns were not being taken seriously. She was also afraid to ask questions, as she was concerned about being seen as a difficult patient.
“At first, I was in denial about my diagnosis. I'd never even considered that I might have a mental illness,” says Charise. “Even after I was discharged from the hospital, I had a really hard time. I was taking my medication, and I felt like that was making me foggy. I was incredibly depressed.”
After attempting to wean herself off her medication, Charise experienced another manic episode and was hospitalized again. This time, her psychiatrist increased her dose of lithium, a medication that can be effective for managing bipolar disorder. Because lithium carries a risk of toxicity – patients must be closely monitored through regular blood tests.
Shortly after her second hospitalization, Charise’s husband was asked by his employer if he’d be willing to transfer to Toronto. Together, they decided a fresh start would benefit their family, so they made the move. Which is when she was referred to the out-patient psychiatry clinic at Mount Sinai Hospital.

Finding compassionate psychiatric care when it mattered most
On that first visit, Charise met with Dr. Mark Halman, a Psychiatrist in Mount Sinai Hospital’s outpatient clinic, who took a complete history and ordered blood work to check her lithium levels. They were dangerously elevated because of how much her dosage had been increased, and she was at risk of developing symptoms of toxicity.
“I was so lucky. Right away when he saw me, he helped me physically. But ever since then, he’s always been so wonderful,” says Charise. “He monitors my lithium levels, answers my many questions, and helped me through the pandemic. He's really made himself available for me based on what he knows my needs are. He’s been fantastic and I haven’t had to be hospitalized since moving to Ontario.”
The level of respect she feels from the team at Mount Sinai Hospital made a significant difference in how Charise receives her care. This commitment to establishing trust and supporting patients as they navigate their health-care journeys is at the heart of what the Psychiatry team at Sinai Health aims to accomplish, and not just with outpatients like Charise.
Excellence in Psychiatric care at Sinai Health creates pathways to partner with other institutions
The Psychiatry team is integrated into a variety of programs and clinics across both Mount Sinai and Hennick Bridgepoint Hospitals. Whether they are assessing and treating psychiatric illness, helping individuals manage the complex intersection of physical and mental illness, or supporting caregivers who are navigating a loved one’s journey with dementia, this team of experts is committed to providing compassionate, patient-centred mental health services across the breadth of programs and clinics at Sinai Health.
“We pay a lot of attention to how to build a strong therapeutic alliance with our patients and how to maintain it. Because essentially, without an alliance, you can’t do medicine. You can’t actually help anybody if you aren’t agreeing on your goals,” says Dr. Bob Maunder, Interim Chief of the Department of Psychiatry, Head of Psychiatric Research and Chair of Health and Behaviour at Sinai Health.
Mount Sinai’s reputation for excellence in Psychiatric care has created opportunities to collaborate with other hospitals, developing better care pathways for patients in need of both physical and mental health support. One program, implemented in partnership with Sick Kids, helps support young patients through the often challenging transition into adulthood as they take on more of the responsibilities of managing their health conditions.
Another partnership, with CAMH, creates formal referral pathways for adult patients with significant mental health needs who also require attention for their physical health. If admitted first to Mount Sinai, the hospital will care for them until they are well enough to transition over to CAMH to continue to care for their mental health. Similarly, if a patient is first admitted to CAMH but has significant physical health needs, that patient will be transferred to Mount Sinai, where they’ll receive ongoing mental health care throughout their medical treatment. These partnerships reflect Sinai Health’s deep commitment to providing integrated care tailored to individual patients’ needs.
Turning experience into advocacy to help break down stigma
Another way Sinai Health maintains its focus on the patient experience is through Patient and Family Advisory Committees (PFACs). These groups – which are made up of staff, patients and caregivers – meet regularly to discuss policies and procedures that could impact patients, and the participants share input. Charise now sits on the PFAC for Mount Sinai Hospital, as well as the PFAC for the Psychiatry Department.
“I see it as giving back, but I also see it as something that's helpful for me,” says Charise. “It makes me feel like some of the challenges of living with a mental health condition are worth it if I can help other people who might be going through something similar.”
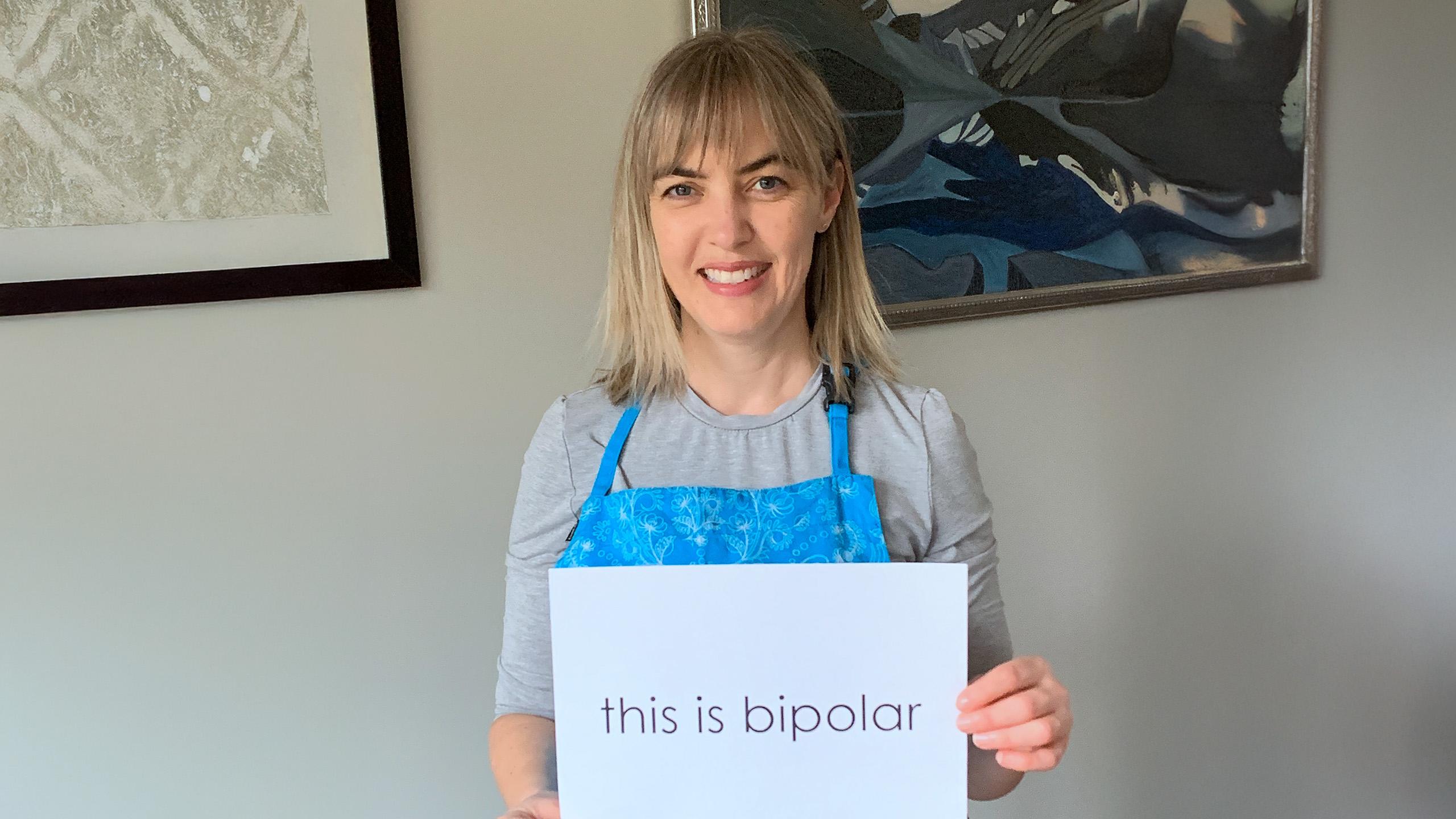
Charise has also channeled this desire to help others into her work as an author. She’s written three books that each seek to raise awareness and reduce stigma around living with a mental health condition – one is a memoir about her own health journey. For her, it’s an important way to reduce the shame that can still come with a mental health diagnosis.
You can support life-changing mental health care
When you support Sinai Health, you make it possible for us to continue developing integrated programs that provide meaningful mental health care to patients when they need it most. Make a gift today to make a difference in the lives of patients like Charise.








