A deep dive into acute care for a pregnant COVID-19 patient
In early 2021, Mount Sinai Hospital began seeing more pregnant patients with COVID-19. One of those patients was Janice Nguyen, who at 23 weeks pregnant contracted COVID-19 and was admitted to Mount Sinai’s ICU and spent weeks on a ventilator. Janice had to learn how to walk and talk again before heading to Hennick Bridgepoint Hospital for the next phase of her care journey.
To learn more about the acute care stage for Janice, we spoke with three members of the care team at Mount Sinai: Nick Bradley, Physiotherapist, Shona Sen, Occupational Therapist and Darcy Roza, Speech-Language Pathologist.
Tell us about your role in Janice’s care
Nick: I became involved following extubation. A CT scan revealed that she had a cerebellar stroke, and once we knew that, we knew how to approach her physiotherapy. We started with simple exercises to get her shoulders and hips moving again and to gain her strength back. We then worked on sitting up on the edge of the bed, which was a challenge because it was tough for Janice to find her balance. A couple of weeks after learning how to stand again, we worked on steps. Once she was discharged from the ICU, I followed her to the maternity unit to continue rehab.
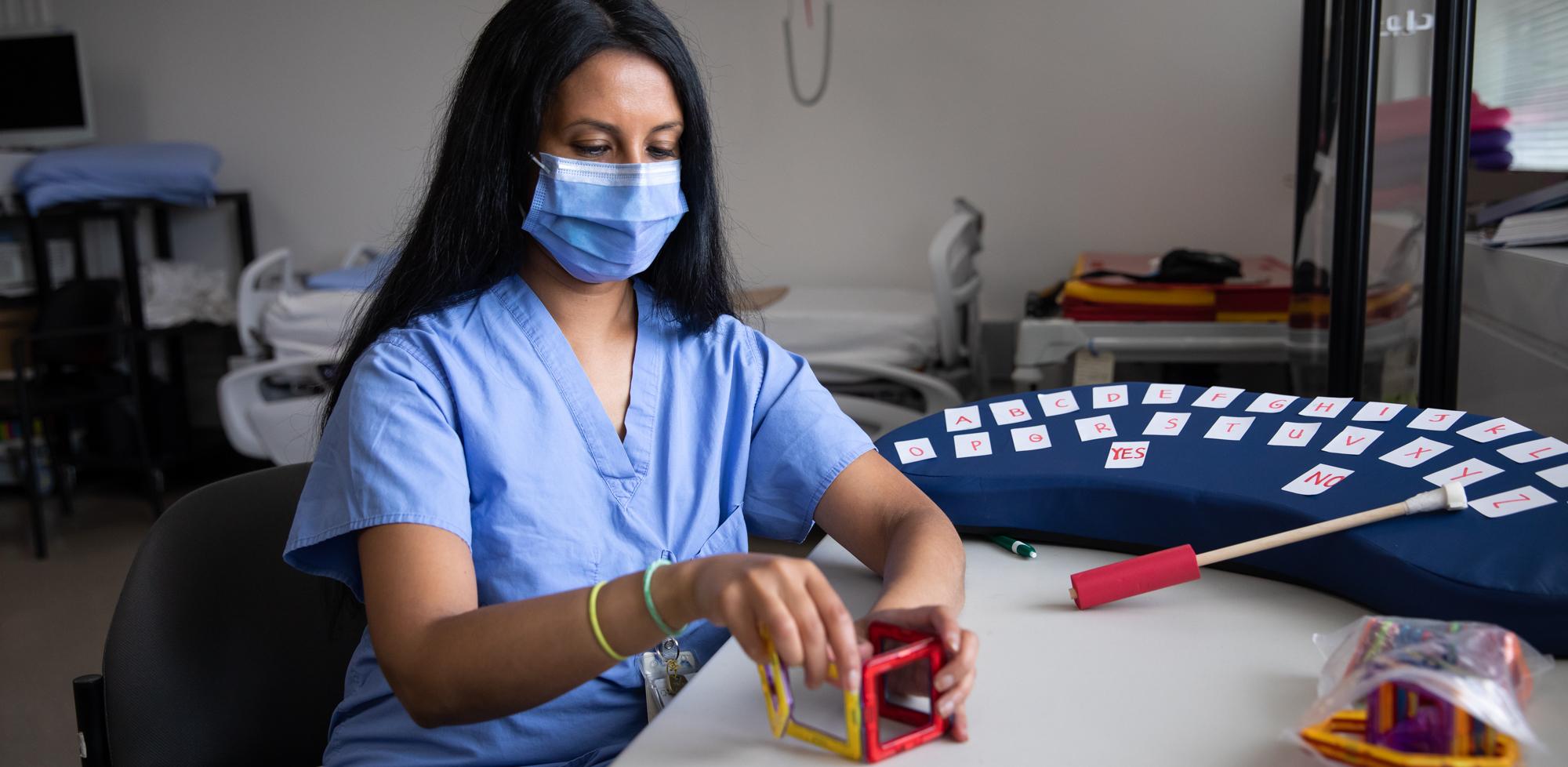
Shona: The first time I met her, Janice wasn’t able to speak. When communicating, she would wiggle her foot to indicate “yes” or “no”. I created a device to help her communicate; we took a bed wedge and put letters on them so she could spell out words. She used a pointer stick to point to letters. Eventually, we worked on positioning, sitting balance, upper body range of motion and motor skills. Janice loves arts and crafts, so we were able to use art modalities in her therapy to work on fine motor tasks. We set up an easel so that she could use her full arm for paintings.

Darcy: As a Speech-Language Pathologist, I focused on how her care team could support her from a swallowing and communication perspective. Janice was unable to swallow and was not receiving any nutrition by mouth. I completed swallowing assessments and slowly transitioned her to eating and drinking by mouth and eventually to regular textures. In terms of communication, I first met Janice when she was only communicating using her feet to signal ‘yes’ and ‘no’. I completed communication assessments and had a lot of joint sessions with Shona to ensure Janice understood everything about her care. I also helped develop a communication book for Janice. If she said a word that nobody understood, she could point to it in the book to minimize any communication breakdowns.
Janice’s case required a lot of collaboration between teams, how did you collaborate across others units?
Darcy: Because Janice couldn’t swallow, my team performed a video swallow study. This was particularly challenging because she was pregnant at the time – I don’t believe we’ve ever performed this study on a pregnant patient in the past. There was a lot of collaboration with both Nick and Shona’s teams to ensure Janice was comfortable in the special speech chair for the study.
Nick: This was quite a unique case at the time and some of the nurses in the ICU were working with equipment they hadn’t previously used, such as the overhead lift used to get Janice to her bed safely.
Shona: For me, I collaborated with the Occupational Therapist in the Neonatal Intensive Care Unit, where Janice’s daughter Flora spent some time after her birth. We collaborated on ways Janice could hold Flora comfortably while she was continuing her therapy. The main takeaway for me from a collaboration perspective, is that we all needed each other so much. Our entire goal for rehab is to create that independence for the patient. I truly believe we couldn’t have done it without each other.
When it comes to treating COVID-19 patients, not a lot of people know about the care involved. What would you want those people to know about the acute care stage?
Shona: Acute care can be hard! Not just for the patients, but the care team as well. With all the different COVID-19 cases we’ve seen, rehabilitation during the acute care phase can be very difficult, and people may not realize that. People may hear about COVID-19 patients being admitted to the ICU, but know so little about the post-ICU acute care stage and how hard it is to get patients in a position to leave the hospital.
Darcy: Exactly. No one know what happens between intubation and rehab. Many patients are confused, delirious, or can’t sit up, walk or swallow and eat. And not everyone gets to go to rehab.
Nick: The general population looks at COVID-19 as survivability, and are not aware of the hospitalization process, such as dialysis or intubation. Janice’s case is just one example of the resilience that is required from both the patient, their family and the hospital care team.
This month, Janice had the opportunity to reunite with a few members of her care team, who she hadn’t seen in a year. See below for some photos from the touching reunion.
























