A built-in killer switch eliminates dividing cells from lab-grown transplant tissue to improve patient safety
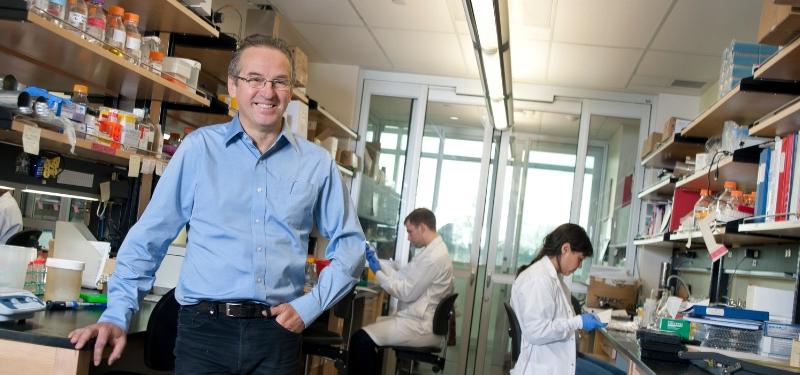
Cells hold great potential as medicine but they can’t be trusted in their current form. “Cells that can divide are dangerous by their nature,” says Dr. Andras Nagy, Senior Investigator at Lunenfeld-Tanenbaum Research Institute, referring to cells’ ability to mutate and spark cancer.
The same is true for tissue that has been derived from stem cells—embryo-like cells that can turn into any other cell type in the body. Researchers across the world are trying to grow stem cell-derived replacement tissue to treat disease. But, there’s a real risk that a graft made this way could unwittingly introduce into the body dividing cells that could wreak havoc.
“The first principle in medicine is not to cause harm to the patient,” says Nagy, who’s dedicated his life’s work to creating useful cells for therapy and holds Canada Research Chair in Stem Cells and Regeneration. “As cell therapy moves into clinical practice, we must avoid causing harm by this new medicine.”
That is why Nagy has developed a remotely controlled killer switch for eliminating potentially dangerous cells during cell therapy, as described in a study out in Nature. The switch is introduced into stem cells which are then coaxed to turn into the desired cell type.
Dubbed the “Safe Cell” system, and four years in the making, the technology selectively wipes out any dividing cells that could potentially cause problems down the line. Its main component is the genetic killer switch that is turned on by ganciclovir, a widely used drug that can be added to the cell graft before or applied directly into the body after the transplant.
“These engineered cells are safer than our own cells which we have no way of stopping if they go bananas and start dividing,” says Nagy, “But if one of the engineered cells becomes tumorigenic, ganciclovir acts as chemotherapy that’s very specific for the implanted cells only.”
To show that it works, the researchers implanted into the mouse eye a piece of lab-grown retina sprinkled with dividing stem cells, both of which contained the killer switch. Upon injecting ganciclovir into the eye, the dividing cells disappeared. Without the drug, however, multiplying cells began spreading across the eye within days. This can cause severe damage, as when a patient reportedly went blind last year in the US after stem cells were injected into her eye as part of a dubious treatment in an unlicensed clinic. Fortunately for the mice, later drug injections eliminated the proliferating cells without affecting the graft or the surrounding tissue, meaning that the killer switch has the potential to safeguard safety in patients too.
Importantly, the Safe Cell system allows researchers to calculate for the first time the likelihood of things going wrong with cell therapy.
“To make an informed decision, it’s important to know how much risk is involved. Driving is risky, but we still do it because the odds of something bad happening are low. But for cell therapy, the level of risk has been unknown—until now,” explains Nagy.
By growing vast numbers of cells with the built-in killer switch, the team was able to calculate the odds of rogue cells appearing—cells that have lost the switch and can multiply in the presence of ganciclovir.
As expected, the chance of this happening was lower when fewer cells were involved. Depending on the disease, cell therapy may require anywhere from a hundred thousand cells to treat blindness to 10 billion cells that would be needed for heart repair.
Knowing the level of risk for each type of therapy will allow clinicians and regulatory bodies to make informed decisions about patient safety.
“We think that our ability to quantitate the risk is going to have a major impact on the future cell therapies because we can make this decision properly,” says Nagy.
Nagy says the killer switch is “fail safe” because it is composed of two genes, where one is required for the division while the other triggers cell suicide. The genes are stitched together in the genome so that they are turned on at the same time. If a cell starts dividing, this will cause its death so long the drug is there to flip on the switch. And it’s extremely difficult for the cells to develop resistance to the drug because if they lose the switch, they also lose the ability to multiply.
After growing billions of cells—as many as humanly possible for an academic research lab—without seeing any rogue cells appear, the team turned to computer simulation to test the limit of the Safe Cell system. The algorithm ran nonstop for four weeks to complete the task of growing trillions of virtual cells. This time, a few rogue cells turned up. But the odds were small and further mathematical modelling revealed this could be avoided by the addition of a second killer switch into the cells.
The researchers also hope the Safe Cell system will help curb another unwanted growth—that of unregulated stem cell clinics offering untested treatments that harm people.
“Regenerative medicine has enormous potential but as this technology begins to enter the clinic it is essential to ensure it is as safe as possible for patients,” says Jim Woodgett, Director of Research at the Lunenfeld-Tanenbaum Research Institute. “We believe this research will have a broad impact on medical use of stem cells.”
“With this kill switch as a safety system, we can begin to contemplate further modifications to transplanted cells, say to evade the immune response— a central challenge in regenerative medicine and something we could not even imagine without this fail safe protection,” says Michael Sefton, Executive Director of Medicine by Design which partly funded the study.
The study was funded by research grants from the Canadian Institutes of Health Research, Medicine by Design and The Foundation Fighting Blindness. The Safe Cell technology has been licensed to panCELLa, a company developing solutions based on regenerative medicine.
Written by Jovana Drinjakovic