Supporting patients during one of life’s biggest transitions

Patients on Bridgepoint’s Transitional Care Unit face one of the biggest challenges that comes with getting older—losing independence.
Most of the patients on the unit are older adults who have experienced a change in their health and can’t go back to living in their previous homes. Over the past year, employees on the unit have been working on a series of quality improvement projects to enhance care and support for patients as they prepare to make the transition to a new home in long-term care or assisted living.
Leo Alfaro, Patient Care Manager on the unit, says patients are typically admitted after a stay on an acute care or inpatient rehabilitation unit. Although they no longer need the higher level of care provided in these settings, they still need care and support. “Most of our patients have complex health conditions and many use a wheelchair or walker. More than 70 per cent have some kind of cognitive impairment and many of these patients experience behavioural and psychological symptoms of dementia. Often patients on the unit need support or assistance for day-to-day activities such as eating, dressing or bathing.”

Georgi Georgievski, a Social Worker on the Transitional Care Unit, says the team worked together to enhance programs and supports to meet the unique needs of this patient population. “For these older adult patients staying in the hospital while waiting for a place in long-term care, there is a risk of deconditioning or decline in physical function and cognitive function. To add to that, in this time of transition, patients and families often have feelings of grief and loss as they cope with this major change in their lives,” he says. “We started this project with the question of how can we maximize our patients’ opportunities to be physically active, socially and cognitively engaged and emotionally supported to try to ease this transition?”
The team took a holistic approach to the quality improvement project, examining care delivery from many different angles. Some examples of improvements included:
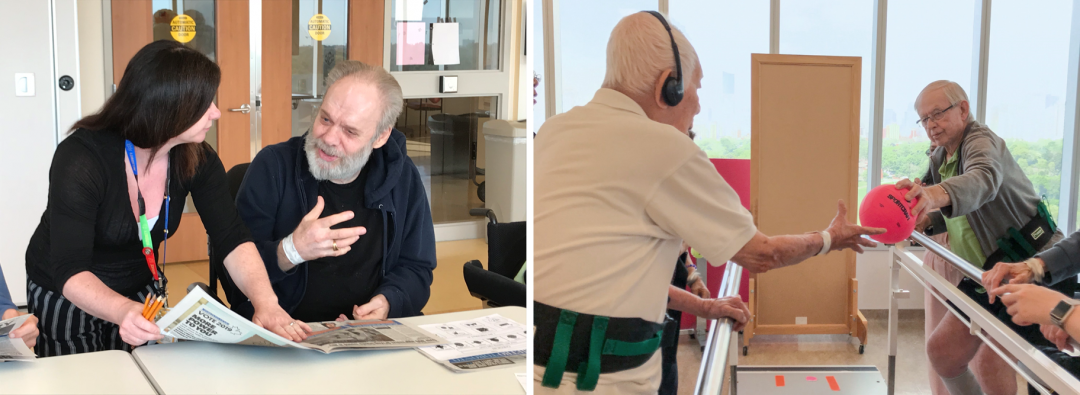
New group exercise classes to help patients maintain physical function in a welcoming social setting.
More opportunities for cognitive and social engagement in group activities, like baking, a “Brain Boost” group program and a program where participants reminisce together. A new volunteer program was also launched on the unit, with volunteers specially trained to engage with older adults.
Enhanced support for family caregivers with a new “relax and chat” group and increased one on-one-counselling with a social worker.
Education for the care team to support them in managing the behavioural and psychological symptoms of dementia, including specialized training, team huddles focused on behavioural symptoms and learning from case studies in a new behavioural rounds series.
The teams have implemented and evaluated these projects and have seen a significant benefit to patients and families. “Through these projects we have seen more patient participation in physical activity and physiotherapy. Patients have also reported a greater sense of well-being,” says Georgi.
Florence Gumahad, a Physiotherapy and Occupational Therapy assistant says she can see the physical and psychological benefits in the exercise groups she leads. “I often see patients become more interested in how their bodies move and in doing activities of daily living and physiotherapy. For me it’s so fulfilling when patients can also see physical changes and changes in how they feel. That has an impact on their quality of life and their goals for the future.”