The story behind the Schwartz/Reisman Emergency Medicine Institute

The Schwartz/Reisman Emergency Medicine Institute (SREMI) is at the forefront of transforming emergency medicine in Canada. Not only for front-line providers but for patients who often have nowhere else to go but the emergency department (ED).
With more than 40 ongoing projects collecting data to better understand the needs of ED patients, to care models that have been replicated nationally and internationally, the team at SREMI is on a mission: to create evidence to guide practice, and to put that evidence into practice.
Why? Because the status quo isn’t enough.
Our job is not just to care for patients. Our job is also to be thought leaders, and to evaluate and create better ways we care for people. SREMI is one of the best places in Canada for emergency physicians to do that kind of work.
How it all started
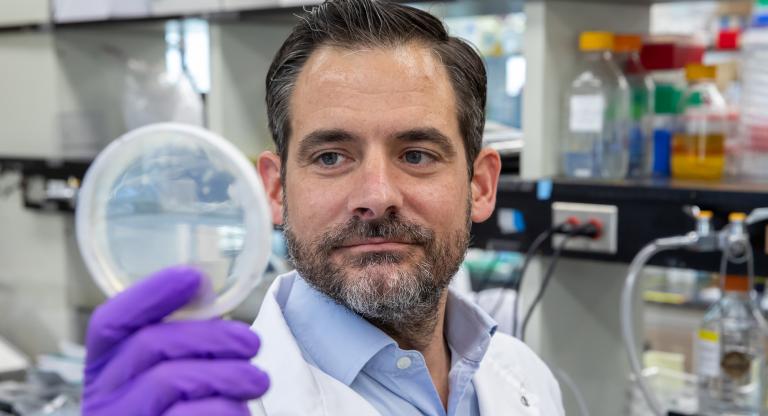
Dr. Borgundvaag is an emergency physician and knows firsthand the unique challenges EDs face. Ten years ago, he was given the opportunity to go “create something” that could help improve the way EDs operate and serve their patients.
To better understand this, he says we have to look back at history and the evolving needs of patients.
Emergency medicine was established in the 1980s. It was first designed to treat acute, life-threatening conditions like heart attacks and trauma. But over time, patients started needing care for increasingly complex and chronic problems, and many groups of patients started relying almost exclusively on EDs.
“Beyond simply providing care and calling it a day, how do we figure out what high-quality care looks like? And what is the most efficient way to organize care in EDs for the unique patient populations we see?” said Dr. Borgundvaag.
That’s where SREMI comes in. SREMI is a not-for-profit research, education and health policy institute. It leads and supports a community of clinicians, researchers and educators to focus on the issue of improving emergency care in Canada and beyond.
A partnership between Mount Sinai Hospital and North York General Hospital, SREMI brings together academically minded emergency physicians to figure out where some of the biggest gaps, and the most pressing issues lay in ED care.
As Canada’s only institute of emergency medicine, their strategy has been to collect real-world empirical evidence on treatments and outcomes in ED patients, and to design ways to make ED care more patient centered, efficient and resulting in better patient outcomes.
SREMI’s areas of focus
Specific areas of focus for Mount Sinai include complications seen in the first trimester of pregnancy, care of older adults, cancer patients and those with mental health and substance use disorders. The focus at North York General has been care of refugees and newcomers to Canada.
One project that was born through SREMI is a virtual program at Mount Sinai that was launched last year to improve care for patients experiencing pregnancy loss. With 40 per cent of women experiencing bleeding or cramping in the first trimester of pregnancy and 20 per cent of women experiencing miscarriage, EDs are often the exclusive source of care for this patient population.

Research by Dr. Catherine Varner, SREMI Scientist and Deputy Director, shows that even in obstetric focused hospitals, a significant number of ectopic pregnancies —when a fertilized egg implants itself outside of the womb — and miscarriages are being missed, which can be fatal, highlighting the need for recognition, training and care.
Another important focus area is the care of older patients in the ED. With an aging population, and more seniors are relying on the ED for care. Dr. Don Melady, who
leads Geriatric Emergency Medicine at SREMI, and one of the founding fathers of the
discipline, was among the first to recognize the specialized care needed by geriatrics patients. This work has led to the development of new models of care, such as the role of Geriatric Emergency Medicine (GEM) Nurses, and new knowledge on how to minimize the risk of developing delirium.
Additionally, SREMI focuses on the evaluation of government policies and innovations that impact patient care. Dr Shelley McLeod has been involved in evaluating Ontario’s electronic triage tool (eCTAS), as well as the effectiveness of virtual urgent care which was deployed across the province during the COVID pandemic.
Looking to the future
“The creation of SREMI, and the innovative work that the Institute has allowed us to do over the last decade wouldn’t have been possible without the support of our founding benefactors Heather Reisman and Gerry Schwartz, Mount Sinai Hospital’s leadership, our foundation and the collaboration of clinical colleagues who are willing to go above and beyond to provide better care for the patients they serve,” said Dr. Borgundvaag.
“We are so fortunate to work where we do,” he added. But the work of improving emergency care is challenging on many levels. Looking to the future, he hopes to put more evidence-based models of care into practice.
Because at the end of the day, that’s what it’s really about. Making sure that patients are getting the highest quality of care, when they need and in the best possible way. When patients leave our hospital, I want them to know that we tried, we care and they matter to us.
To learn more about SREMI and the work they do, visit: https://sremi.ca/