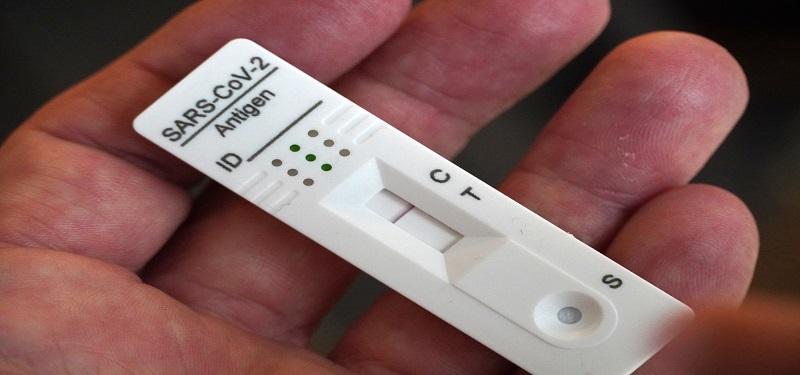
Everything you need to know about rapid antigen tests
In testing, it’s the gold standard. “Polymerase chain reaction (PCR) testing is the most sensitive and it can detect even the smallest amount of the COVID-19 virus,” notes Dr. Jennie Johnstone, Physician Lead, Infection Prevention and Control at Sinai Health.
“This test will always be essential in health care settings for patients and employees.”
Rapid antigen tests can play a role in minimizing the spread of COVID-19 for a specific subset of the population. Dr. Johnstone discusses the uses and clears up some misconceptions about these tests.
Asymptomatic screen testing
Asymptomatic screen testing is a strategy of systematically and consistently using rapid antigen tests during times of high COVID-19 prevalence, to try and identify COVID-19 before you become symptomatic. According to the Science Advisory Table brief released on February 10, with the Omicron variant, you need to test yourself three to five time per week for this to be effective as a prevention strategy. When someone does test positive they can stay home from work or school and limit the spread.
Diagnostic testing
This is when people with symptoms, who are not eligible for PCR testing use the rapid antigen test to diagnose themselves with COVID-19. When people develop symptoms compatible with COVID-19, they require two consecutive negative rapid antigen tests, separated by 24-48 hours, to end self-isolation. Right now, because there is still a lot of COVID-19 in the community, a positive test is considered positive. It is important to note that healthcare workers in the hospital can’t rely on rapid antigen tests to rule out COVID-19 if they have symptoms, as the rapid antigen tests are not as good as PCR.
The one-off
This is when people use these tests before they go to a party or gathering. Rapid antigen tests add a layer of protection, but a negative test should not be your deciding factor about whether you will attend the event or not. It important to note, that one-off rapid antigen testing in asymptomatic individuals without a known exposure to COVID-19 and outside of asymptomatic screen testing programs is not currently recommended by the province. Instead, you should make the decision about attending based on who is at the event, how many people will be there, whether it is indoors or outdoors or if there will there be any immunocompromised people there. Ask yourself if you are okay with COVID-19 being transmitted there and then you may consider performing a rapid antigen test as a layer of protection.
“It’s important to know that having a rapid antigen test come back negative does not mean that you don’t have COVID-19,” notes Dr. Johnstone. “There are a few reasons why the rapid antigen test may provide you with a false negative, including that these tests have a lower sensitivity to the virus, you didn’t do the self-collection properly or because you were negative when you preformed the test, but became infectious moments later.”
If your rapid antigen test comes back positive, since there is a lot of COVID-19 circulating in the community, a positive test is currently considered positive.












