Coronavirus antibodies last at least three months after infection, study suggests
Coronavirus antibodies can last at least three months after a person becomes infected with the virus that causes COVID-19, according to a new study published Thursday in Science Immunology.
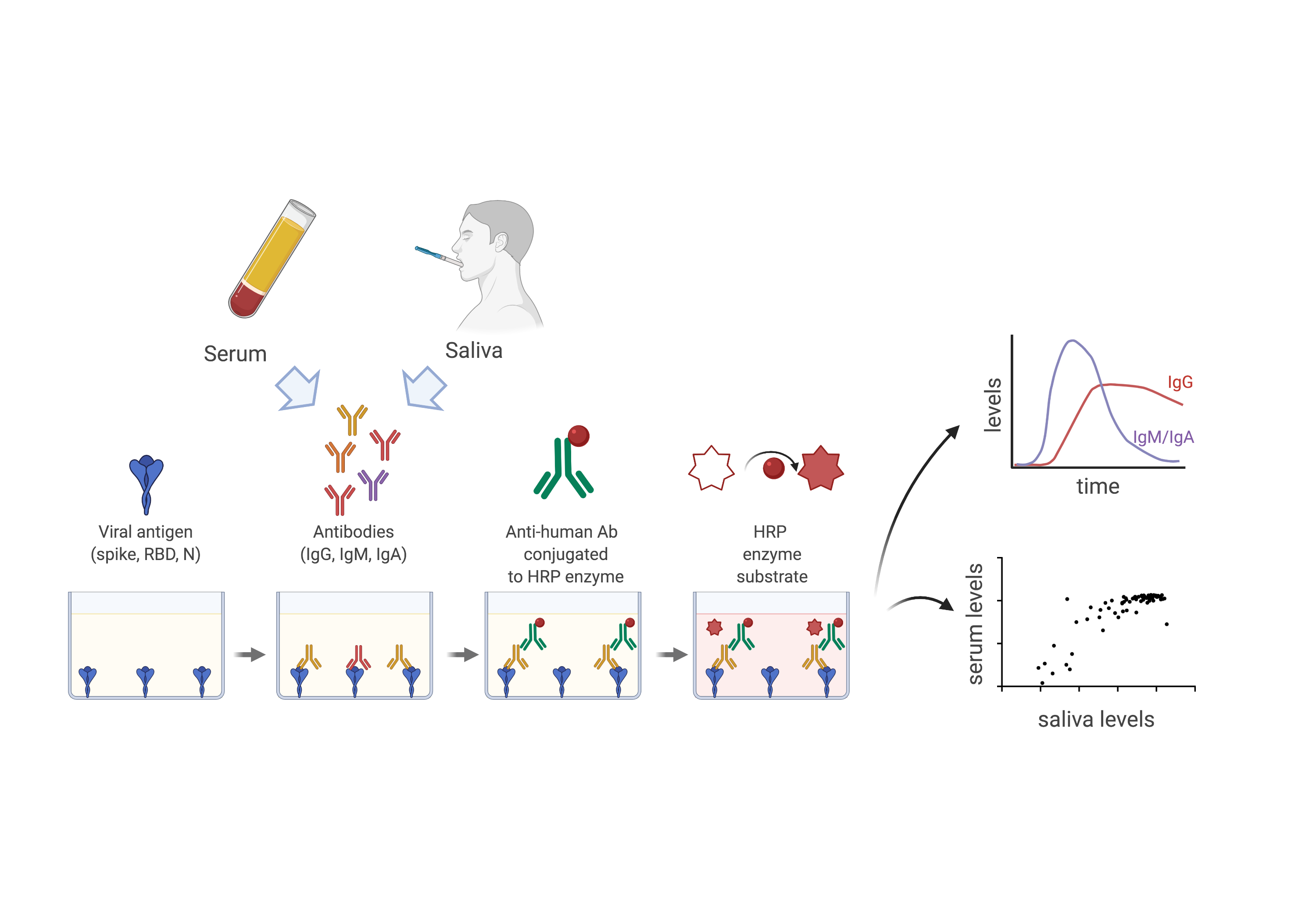
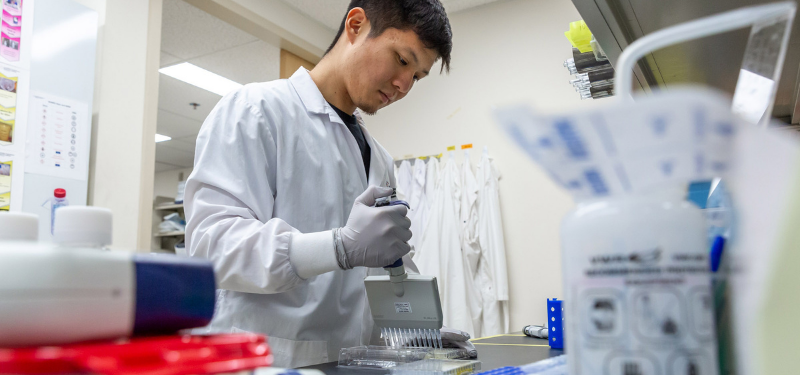
Researchers from the Lunenfeld-Tanenbaum Research Institute (LTRI) at Sinai Health and the University of Toronto used both saliva and blood samples from COVID-19 patients to measure and compare antibody levels for over three months post-symptom onset.
They found that antibodies of the IgG class that bind to the SARS-CoV-2 spike protein are detectable for at least 115 days, representing the longest time interval measured. The study is also the first to show these antibodies can also be detected in the saliva.
“Our study shows that IgG antibodies against the spike protein of the virus are relatively durable in both blood and saliva,” said Jennifer Gommerman, professor of immunology at the University of Toronto and leader of the saliva testing effort. “Our study suggests saliva may serve as an alternative for antibody testing. While saliva is not as sensitive as serum, it is easy to collect.”
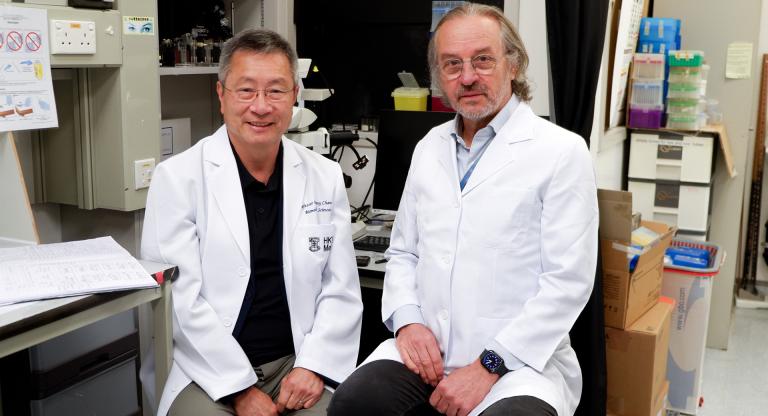
Anne-Claude Gingras, senior investigator at the Lunenfeld-Tanenbaum Research Institute, led a team of scientists that executed the serum assay at Mount Sinai Hospital.
The saliva assay was developed at the University of Toronto, while a team at LTRI, led by senior investigator Anne-Claude Gingras, a professor of molecular genetics at the University of Toronto, executed the serum assay.
“The LTRI platform for detection of antibodies in serum, or blood, is incredibly robust and well suited for assessing the prevalence of infection within the community,” said Gingras. “This is another tool that can help us better understand and even overcome this virus.”
Most people who recover from COVID-19 develop immune agents in their blood called antibodies that are specific to the virus. These antibodies are useful in indicating who has been infected, regardless of whether they had symptoms or not.
A large team of scientists collaborated on the study. Dr. Allison McGeer, a senior clinician scientist at LTRI and principal investigator of the Toronto Invasive Bacterial Diseases Network, along with Dr. Mario Ostrowski at St. Michael’s Hospital of Unity Health Toronto provided access to the paired saliva and serum samples from dozens of patients for the study.
The study was co-led by graduate students Baweleta Isho, Kento Abe, Michelle Zuo and Alainna Jamal. Dr. James Rini, a professor of biochemistry and molecular genetics at the University of Toronto, and Yves Durocher from the National Research Council of Canada provided key protein reagents for the saliva studies.
The durability of the antibody response to SARS-CoV-2 has been debated in recent months. An earlier study published in Nature Medicine suggested the antibodies can disappear after two months for some individuals who had the virus but did not experience symptoms.
This study led by the Toronto team is in agreement with findings from leading immunologists in the U.S. in describing the antibody response as longer lasting.
While the team admits there is a lot they still don’t know about antibody responses to SARS-CoV-2 infection, including how long the antibodies last beyond this period or what protection they afford against re-infection, this research could have broader implications in the development of an effective vaccine.
“This study suggests that if a vaccine is properly designed, it has the potential to induce a durable antibody response that can help protect the vaccinated person against the virus that causes COVID-19,” Gommerman said.
This study was supported by an Ontario Together grant and funding from the Canadian Institutes of Health Research. Funding for the development of the assays in the Gingras lab was provided through generous donations from the Royal Bank of Canada (RBC), Questcap and the Krembil Foundation.