Interactive tool helping health systems around the world plan for COVID-19

How many ICU beds are left in Spain? What about ventilators in Ontario? How many critical care beds are being used in China?
An online tool created by a team of Toronto scientists is helping hospitals and health systems get the answer to these and other questions.
The COVID-19 Acute and Intensive Care Resource Tool, or CAIC-RT, launched Tuesday. The project was led by a group of researchers at the University of Toronto’s Dalla Lana School of Public Health.
The interactive online tool helps key decision-makers estimate their capacity to manage new cases of COVID-19. In 48 hours, it has been used in more than 60 countries and 486 cities across five continents.
Matt Warkentin, an epidemiologist and PhD candidate at Sinai Health’s Lunenfeld-Tanenbaum Research Institute, worked around the clock to code the tool. He estimates the team spent 12 to 16 hours a day getting CAIC-RT up and running.
“It’s been phenomenal. We’ve been blown away,” Warkentin said of the response. “We thought in our heart of hearts that this had potential to be valuable to a lot of people, but I don’t think we had any sense of the scale at which it would blow up.”
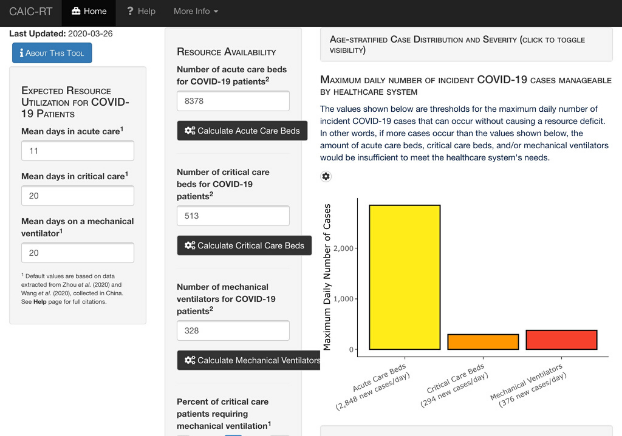
The online tool helps hospitals model their capacity to respond to the fast-moving pandemic by taking into account a number of parameters, including the number of acute and critical care resources available to a specific health system, data on the age distribution and severity of COVID-19 cases and expected duration of patient stays.
“The tool determines the maximum number of new COVID-19 cases that a health-care system could manage,” said Dr. Nathan Stall, a PhD student at the Institute of Health Policy, Management and Evaluation at the University of Toronto and a physician practising geriatrics and internal medicine at Mount Sinai Hospital.
Dr. Ross Upshur, senior investigator at Sinai Health’s Lunenfeld-Tanenbaum Research Institute and professor in the department of family and community medicine in the Faculty of Medicine with a cross appointment at the Dalla Lana School of Public Health, lauded the tool as the latest example of how Toronto scientists are contributing to knowledge-creation and dialogue surrounding the pandemic.
“We’re now using the best of our capacity and some of the brightest young minds in the country to create tools that will help us create evidence-informed decisions,” said Upshur.
“Not only does it help us understand the dynamics of the pandemic, it helps us to respond. It’s looking at both the public health and clinical capacity side of things. The idea of how these two sectors work together is really germane to our response to COVID-19.”
The team is now fielding requests to translate the tool into more languages. Warkentin said they have received a number of offers to help and they are trying to crowd-source translation efforts to further help make it a global tool.












