LTRI scientists hunting for the perfect rhythm to beat depression blues
When it comes to finding a long-lasting treatment for depression, a team of Toronto scientists say it could come down to finding the perfect rhythm.
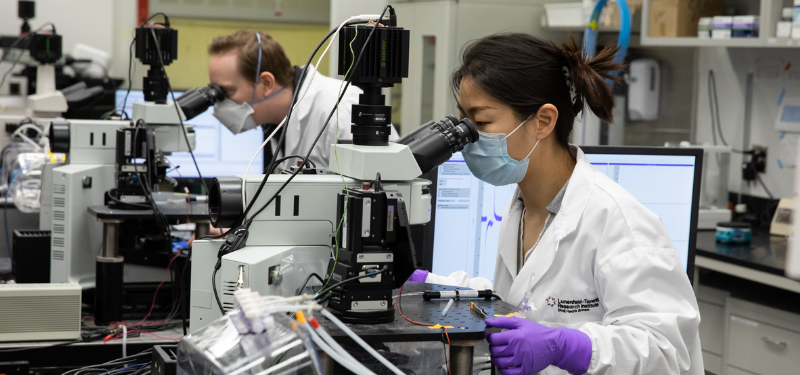
The approach, currently under development by scientists at Sinai Health, the University of Toronto’s Temerty Faculty of Medicine, and the Centre for Addiction and Mental Health (CAMH), has nothing to do with music and everything to do with tweaking an existing form of brain stimulation therapy.
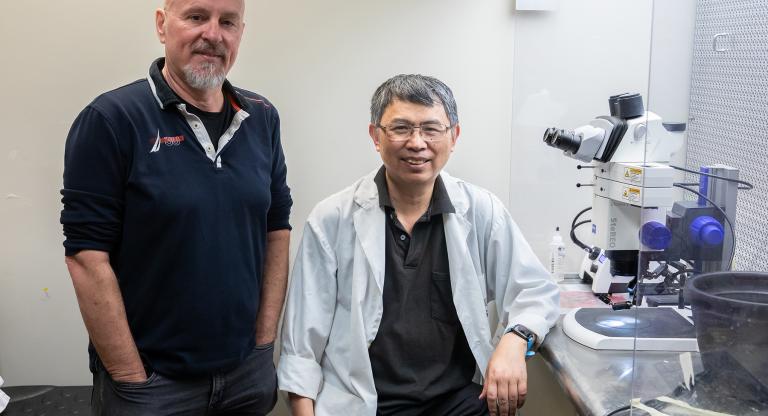
One component is being led by Graham Collingridge, neuroscientist and senior investigator at Lunenfeld-Tanenbaum Research Institute (LTRI) at Sinai Health, alongside LTRI staff scientist John Georgiou. The two are part of a team of Toronto researchers who were recently awarded a grant by Bell Let’s Talk and Brain Canada to not only improve the technology, but also test it on volunteer adult patients.
The research centers around transcranial magnetic stimulation, or TMS, a form of brain stimulation therapy that’s been shown to hold enormous promise in helping patients with treatment-resistant depression. The approach uses a device to deliver pulses of magnetic stimulation to the prefrontal cortex, a part of the brain associated with mood regulation.
In order to find the perfect pattern, the LTRI is collaborating with Dr. Evelyn Lambe, an associate professor in the Department of Physiology at the University of Toronto’s Temerty Faculty of Medicine, who is leading work on optimizing the stimulus parameters in the prefrontal cortex as part of the research grant.
“The ability to rapidly test this new stimulus paradigm in human subjects is based on over 30 years of fundamental research in the field of LTP,” Collingridge said. “It’s impossible to overestimate the importance of basic research for the development of improved treatments for human conditions. If we are successful in our goals, it will be music to my ears.”