Operation move day: Opening the new Kimel Schatzky Intensive Care Unit
On May 10, Mount Sinai Hospital opened the Kimel Schatzky Intensive Care Unit (ICU) , a state-of-the art facility designed to enable clinical teams to deliver outstanding patient-centred care in a safe and comfortable environment.
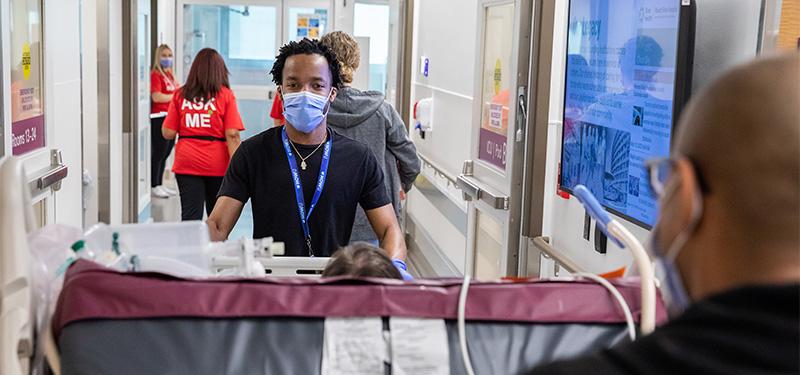
The day also marked the successful and highly intricate move of the Hospital’s critical care patients from their original units to the new ICU.
How do you move critically ill patients spread across three floors in one move day, while ensuring their safety as the utmost priority? Through excellence in comprehensive move planning that puts patients first and enables continuity of care throughout the process.
“Our team has never been fine with being ‘just good enough’. We have always strived for excellence,” says Dr. Christie Lee, Site Director, Critical Care Medicine, of the move to the new ICU. “We strive to make things better for our patients and our families, as they have always been at the center and focus of our care. The ICU is years in the making; the last two years have been an extremely intense time for construction, as well as for operational readiness and planning. We’ve waited a long time for this new space, but our team is ready to care for our patients and their families, and we look forward to the new opportunities ahead.”
Planning was led by the Operational Readiness, Transition Planning and ICU teams, to support patients and caregivers throughout the move and to help settle them into their new space.
Weekly transition meetings, frequent team huddles and the careful scheduling of clinicians to support the move and provide emergency responses for unexpected events such as Code Blues (a hospital announcement signalling a medical emergency) and unplanned admissions were some of the preparations undertaken prior to the move. As was incorporating “lessons learned” insights from other hospital moves, including:
- “Move Team” coloured T-shirts for staff to quickly identify members for support and communication
- Designating a specific role for each care team member for move day
- Boxed lunches and a dedicated break room to allow move teams to stay together to respond quickly to move day requests
The unique process of transporting complex-needs patients to the new ICU was conducted using a pre-determined sequence with two move teams, and a comprehensive patient checklist, detailing each patient’s individual needs related to their acuity (level of the nursing care required), and transport team, monitoring and equipment requirements.
“All aspects of move planning were intended to ensure care could transition as seamlessly and safely as possible from the old to the new ICU,” says Amanda Lachhman, ICU Program Champion, Operational Readiness. “Getting ready to move into a new space with such high degree of changes for the team was a challenging task. We made sure areas such as patient rooms, communication stations, medication rooms and clean supply rooms were set up and ready for providing care. Meanwhile our Biomedical, I.T. and Human Factors teams conducted several rounds of functionality testing with the new technologies, implemented to support patient safety and the monitoring of critical care patients.”
Through seamless coordination, collaboration and an unyielding commitment to safety, patients successfully settled into their modern and comfortable new space.
As part of Renew Sinai, the new Kimel Schatzky Intensive Care Unit is one of many bold, ambitious redevelopment projects that are expanding, improving and transforming the care, facilities and infrastructure at Mount Sinai Hospital.












