Preparing for the future of intensive care
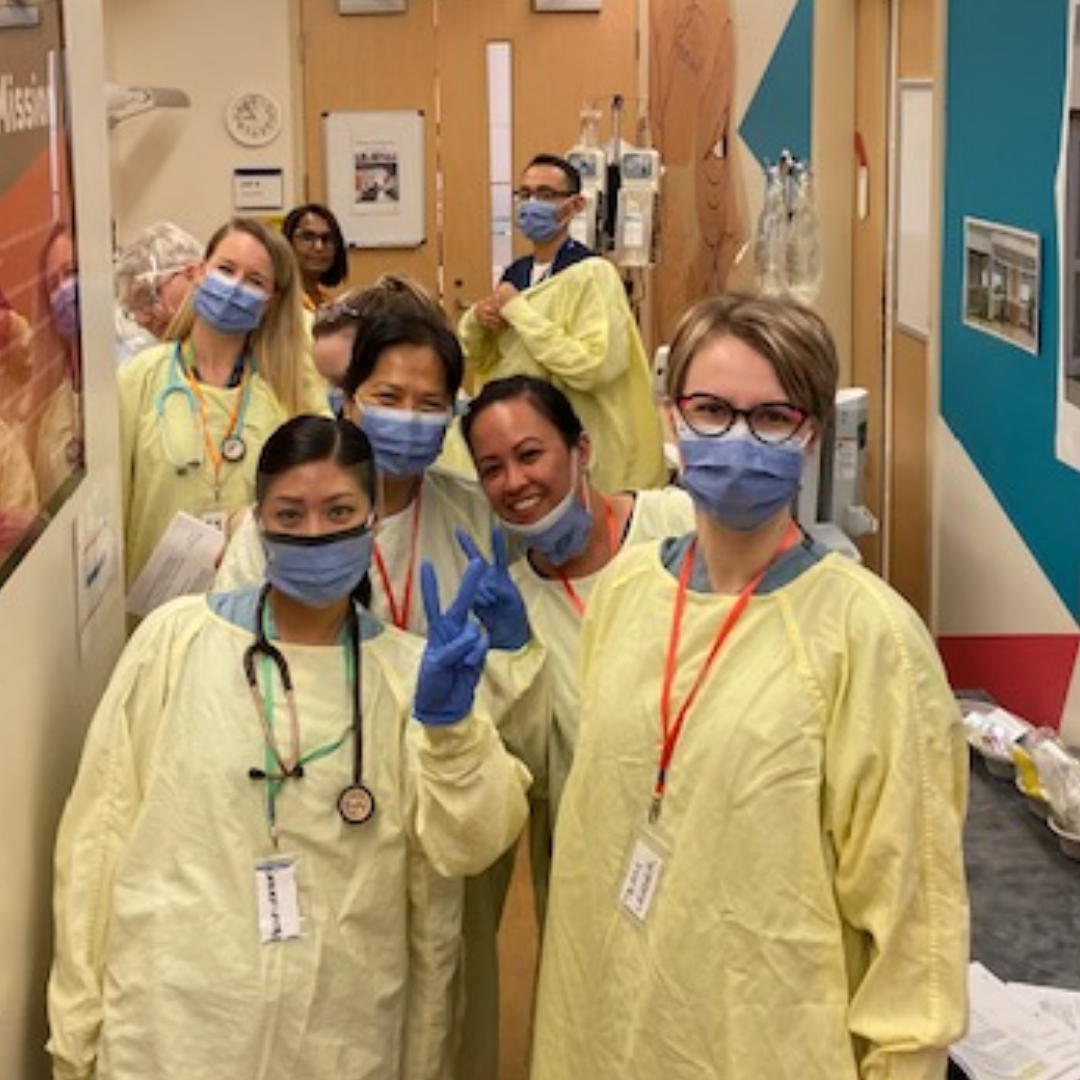
In late January, a number of participants from across Mount Sinai Hospital gathered at the Surgical Skills Lab on Floor 2, in a carefully planned simulation of the new Phase 3A Intensive Care Unit (ICU) rooms.
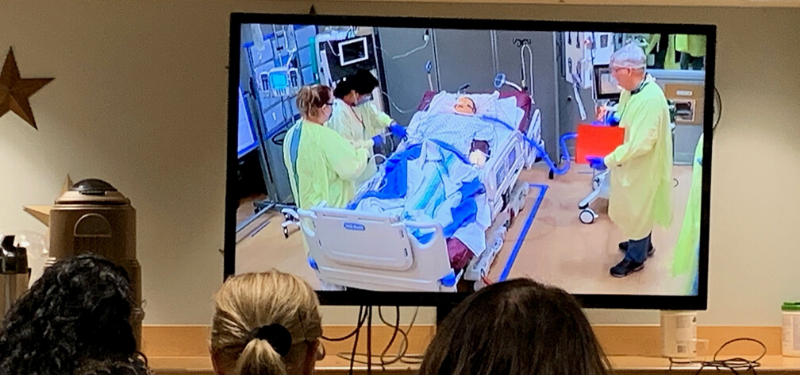
The Surgical Skills lab had been carefully laid out and marked off to specifications that will be found in the new ICU rooms. The simulation room featured boards standing in for walls, pictures showing where windows will be, and two small cabinets replicating the exact dimensions of the new state-of-the art articulating arms. To top it off, there were a number of cameras recording and live-streaming simulated scenarios that had been created to test the limits of the new spaces.
As Mount Sinai Hospital continues preparations to move our ICU from the 18th floor to a renewed space on the fifth floor in 2022, ensuring the new rooms are set up to efficiently treat patients is a vital undertaking led by the Operational Readiness and Transition team.
The floor plans and architectural designs have been available for some time, but it can be a challenge to gain a complete understanding of how two-dimensional drawings will translate to three-dimensional, real-life experiences. That’s why the team from Operational Readiness went to great lengths to really see how critically ill patients as well as their nurses, doctors, respiratory therapists, other care team members and even family members can function together in these new spaces.
“We worked hard to create scenarios that reflected the real-life experiences of our ICU team and their patients,” says Amanda Singh, Program Champion – Operational Readiness and Transition.
While a team of interdisciplinary staff members went through the planned scenarios, other participants watched and listened to a live-stream of the action in the next room. In between scenarios and post-simulation, feedback was collected and debriefing sessions were facilitated by the Human Factors team who will also be analyzing the video footage and providing additional recommendations based on their analysis. “One of the goals of this exercise was for front-line workers to ask questions and find opportunities to improve the space,” adds Jennifer Jeon, Lead, Human Factors and Patient Safety. “The live-streaming allowed for feedback from the larger group of viewers to add their thoughts, as well as hearing from the scenario participants.”
Tanya McDonald, Director of Operational Readiness, noted how exercises like this provide feedback that makes a real difference. “What we are trying to do here is set the gold standard for how we gather feedback from the users of the space; physicians, staff, patients, and their families,” said Tanya. “We place a high value on participant’s honest feedback – it makes a world of difference to the operational readiness of the final space.”
Our new Intensive Care Unit is more than doubling in size, going from 14,600 square feet to a 35,500 feet and will accommodate 36 patients, with rooms that will be set up to accommodate different levels of acuity.
Learn more about the largest redevelopment project in Mount Sinai Hospital’s history here.