Research at The Ontario Fetal Centre to lay solid foundation for groundbreaking medical interventions for spina bifida

Each year in Canada, spina bifida affects approximately 120-150 fetuses. Although not life threatening, babies born with spina bifida may have varying degrees of disability, depending on the location of the spinal defect.
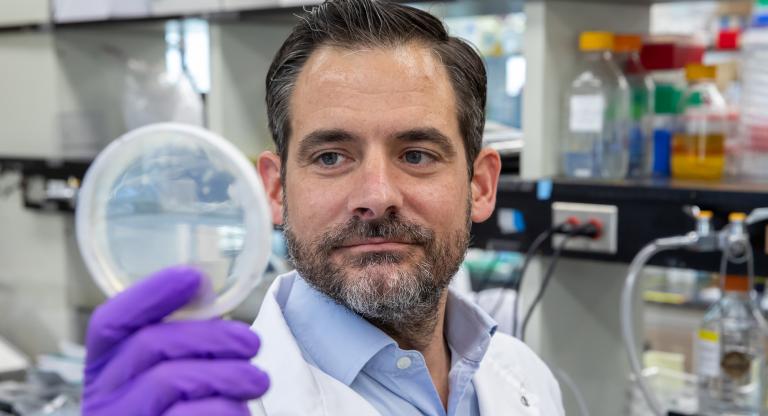
Dr. Tim Van Mieghem and his team at The Ontario Fetal Centre, a partnership between Mount Sinai Hospital and the Hospital for Sick Children (SickKids), are advancing equitable access to high-quality care through a fully funded, three-tiered research project, focusing on prevention, early detection and advancing treatment options.
Prevention
“One known contributor of spina bifida is a lack of vitamins before birth, especially folic acid. Explains Dr. Van Mieghem, maternal-fetal medicine specialist at Mount Sinai Hospital. “But most women in Canada have sufficient folic acid intake through their diet or additional vitamin supplements. What we’re now looking at in terms of prevention, is whether there are other factors that play a role in maybe not folic acid intake, but folic acid uptake in the gut and folic acid production in the body.”
In collaboration with Dr. Kristin Connor at Carleton University in Ottawa, the team is looking into the role of maternal gut microbes and placental transport, by comparing these factors in pregnant people carrying a baby with spina bifida, to those carrying a fetus without spina bifida.
The team hopes to uncover whether differences in gut microbes between these two populations could be a target to prevent and diagnose spina bifida early.
Early Diagnosis
When prevention isn’t possible, early diagnosis is critical to improving pregnancy care. Current ultrasound screening available during the first trimester of pregnancy can diagnose spina bifida early, when sufficient expertise is available. In 2018, the team at Mount Sinai established the Fetal Early Anatomy Clinic to provide advanced diagnostic assessment for high-risk pregnancies, allowing for even earlier detection of fetal abnormalities.
“With new technology in place and high quality ultrasounds, we now have the ability to see different organ systems with a high degree of acuity.”
Although every pregnancy would stand to benefit from this technology, it requires a high level of operating expertise. With this in mind, the team is currently exploring the potential of artificial intelligence (AI) in collaboration with the Vector Institute at SickKids. Funded by a grant from the University Health Network Innovation Fund, a computer algorithm is being trained to detect fetal abnormalities. The goal of this AI program is to interpret these images hopefully to a similar level of quality as a skilled sonographer or radiologist. If this can be achieved and rolled out across Canada, it would diminish barriers with operating expertise and increase access to early diagnosis.
Advancing Treatment Options
The third pillar of research is focused on treatment of spina bifida.
“Ultimately the goal for us is that when we detect conditions such as spina bifida early, we can start counselling patients and treat these conditions even before birth,” explains Dr. Van Mieghem.
Funded by a research grant from the Canada Foundation for Innovation, experimental research is currently underway to assess the advantage of robotic fetal keyhole surgery (fetoscopy) to operate within the uterus. This procedure would eliminate the need for large cuts in the maternal womb and abdomen, in order to operate on the fetus and could potentially reduce other risks associated with in-utero surgical procedures, such as uterine scarring, preterm birth and future complications with childbirth.
Since 2017, Mount Sinai Hospital has been performing in-utero surgery, aimed at decreasing the adverse effects of spina bifida. The Ontario Fetal Centre recently completed their 44th surgery and is the only hospital in Canada to offer this complex intervention.